Functional Neurological Disorders
Pathophysiological Hypotheses
HISTORY
From antiquity to the XIX century
The history of ideas concerning hysteria is very old and is one of the most
exciting in the history of medicine. During Greek antiquity (Hippocrates), the
origin of the disorder was at the level of a "wandering" uterus that could block
the nervous flow and which, for example, could cause respiratory discomfort when
it migrated to the lungs. In the Middle Ages, these patients were often
considered to be witches, cursed by the demon, and could be condemned to the
stake. During the seventeenth century in London, Thomas SYNDENHAM had shown the
protean and changing character of hysteria, with passages from one symptom to
another.
The XIX century
It was not until the middle of the XIX century that its cerebral origin was
recognised (Pierre BRIQUET). This Parisian neurologist proved, of a fashion, the
role that favoured ancient traumatic experiences. A little later, John Russell
REYNOLDS of London showed the importance of emotions and of "ideas" or
representations in the apparition of symptoms (before making a move, it must be
programmed from an idea). Also in the late XIX century, Jean Martin CHARCOT,
neurologist at the Salpêtrière in Paris, attempts to apply the Anatomo-clinical
method of neurology to the hysteria that he will first consider as a purely
neurological problem. He was to issue the very modern hypothesis of "functional
lesion". This lesion, he would not be able to see by analyzing the anatomical
parts of brains of deceased hysterical patients. However, this hypothesis would
be confirmed by recent data from functional brain imaging (see below). Having
not found a functional lesion, he was to gradually abandon the neurological
approach and instead attach importance to emotions and ideas (or
representations, more often unconscious): "An idea can cause paralysis and the
other can cure it." He therefore explains some unexpected improvements or
spontaneous cures. He was to create a laboratory of physiological psychology for
the psychiatrist Pierre JANET who would introduce into concept which what would
become major and which we shall discuss below: The phenomenon of dissociation,
meaning the ability that the brain has to "dissociate", to fragment or to
compartmentalisation, during a strong emotion, which can lead to the different
symptoms that are encountered in FND. For example, amnesia sometimes observed
during a major psychological trauma or sexual abuse corresponds to the exclusion
of certain networks of the memory out of the field of consciousness.
The XX century
The conceptual model that had the most notoriety at the beginning of the XX
century was that of "hysterical conversion", a process that converts an
unbearable psychological distress into physical symptoms in order to soothe
anxiety. Sigmund FREUD altered this concept by moving from unbearable
psychological distress to unbearable sexual impulse. Actually, few neurologists
and even few psychiatrists who care for these patients adhere to this concept..
During the twentieth century, there was a certain lack of interest concerning
the subject of hysteria, in comparison with the development of other
neurological and psychiatric pathologies, both from neurologists and
psychiatrists. There are several possible reasons:
1) During World War I there was a sort of epidemic of hysterical phenomena
amongst soldiers in connection with extreme situations on the battlefield.
Neurologists used barbaric methods trying to treat these patients whom they had
difficulty understanding. Perhaps they wanted to somehow forget this difficult
period (see in the drop down menu "patients"
the text on World War I)
2) Neurologists had difficulty recognising as a "neurological" patient those who
had fluctuating and incongruous symptoms in relation to the symptoms encountered
in classical neurological pathologies. Not complying with the rules of
anatomical-clinical correlations elaborated over several centuries by
neurologists, could be considered unbearable. However, we can see below, in the
examples given of patients, that these so-called "incongruous" symptoms may be
consistent with certain pathophysiological models of FND
3) The considerable development of identification of neurological pathologies
thanks to techniques of imaging, biological examinations, genetics and pathology
has left little room for these hysterical patients who do not allow themselves
to be apprehended by supplementary exams.
CURRENT THEORIES
The beginning of current conceptual change is some ten years old and it was
initiated by our British neurologist colleagues. They studied large series of
patients with FND, their symptoms, triggering modes and their evolution. The
onset of symptoms from a psychological factor is no longer considered as
indispensable. Physical trauma can cause this type of disorder without there
being any associated psychopathology. In these patient series, the overall
prognosis for these disorders is unfavourable even on long-term studies after 12
years. These neurologists consider that paralysis has the same overall prognosis
as multiple sclerosis, that functional abnormal long movements have the same
prognosis as degenerative diseases of grey nuclei, that non-epileptic seizures
have an evolution sometimes more serious than epilepsy itself. They have clearly
shown that treating these patients as suffering from psychiatric pathology only
aggravates the situation. They propose considering these patients as having a
neurological problem with a disturbance of the cerebral "software", without
neglecting the psychological approach necessary in many patients. The term
functional Neurological disorders (FND) was proposed to emphasize the importance
of a neurological approach in patients.
FND is now considered like the consequence of changing brain connectivity (all
the connections between the cerebral neurons). But several explanatory models
currently exist to explain how physical trauma, a medical condition or a
psychological event will produce functional neurological disorders.
1) The Bayesian model
The most commonly accepted model is currently the one developed by Mark
Edwards. It refers to the Bayesian model of brain functioning. The brain
functions as a computer in which is progressively built an internal model of the
world that will permit interaction through predictions from sensory information
the brain will receive. For each information received, there is an anticipation
or prediction through statistical inferences, most often unconscious, on the
nature of this information. In this model, the brain constantly generates such
anticipations. This system saves time by having information in advance. When
these predictions are violated by unexpected sensory inputs, they trigger a
signal of surprise or error. Events triggering functional disorders will modify
the internal model of the world and consequently, alter ideas and predictions
about the information received, resulting in focused attention disorders and
disruption of perceptions and movements. The treatment that follows from this
theory will essentially consist, through cognitive therapy, in trying to
standardise the representations supposed to be the cause of the disorders. (For
more information follow this link
to Dr. M Edward's explanatory video)
2) The "Dissociative" model
There currently exists another theory, less commonly adopted, but
appears more consistent with the supposed mode of action and the results of
magnetic stimulation. This theory was introduced at the end of the XIX century
by Pierre JANET. It refers to a psychobiological process through which, under
the influence of intense psychological emotion or trauma, brain functions will
dissociate, fragment, compartmentalisation and will be at the origin of
different neurological functional symptoms. He calls this phenomenon
"dissociative". This process would be non-lesional (functional) and potentially
reversible. It could be the result of connectivity disorders that are beginning
to be seen in functional imaging in some research centres. The behaviors or
processes we want to perform are cut off from consciousness by narrowing the
field of consciousness (monitoring disorder) or the executive system (control
disorder). We will see below that a trauma, not psychological, but focused
physical is more than likely be at the origin of a dissociative phenomenon at
the level of the corresponding neural networks and in return leads to a
functional neurological disorder.
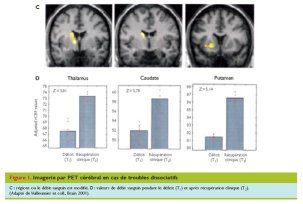
To illustrate this dissociative phenomenon, a study by P VUILLEUMIER in Lausane
shows that in functional unilateral sensory-motor deficits, there exists a
hypoactivity of the cortico-subcortical loops of the contralateral central
region, which disappears once the patient is healed.
Another study by V. VOON in London showed that, in this type of patient, there exists a disconnection between the supplementary motor area which is very important in the programming of movements and the prefrontal regions, causing an inhibition of the voluntary motricity. There is, however, hyperactivity of the limbic regions (emotional brain), reflecting the importance of psychological phenomena in many of these patients.

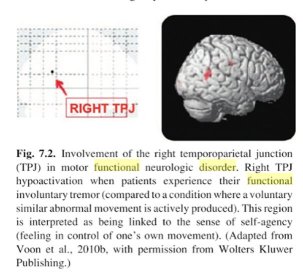
The same researcher showed a disfunction as hypoactivation at the right temporo-parietal junction responsible for agency, a process by which we are aware that the activity we are carrying out was planned by us, and that it belongs to us.
FND are often referred to as
"functional and dissociative neurological disorders". The meaning of the word
dissociative given at present to these disorders is different from that proposed
by P. JANET. In current useage, it refers to states where the subject may be
disconnected from their body and experience a sense of depersonalisation (it
feels weird, disconnected, being both there and not there). He also refers to
states where the subject can be disconnected from their environment and
experience a sense of derealisation (their entourage seems far away and unreal
as if it were hovering. They feel distant from their surroundings.) For Pierre
JANET, all the symptoms of FND are related to dissociative processes.
In this model, it is possible that cross-cranial magnetic stimulation "large
field" and peripheral can act on these connectivity disorders and restore normal
cerebral functioning.
3) The Proprioceptive Disorder model
Research on factors predisposing to FND has focused solely on the
psychopathological characteristics of patients. In this model, FND would be
essentially the result of an activation deficit of peripheral proprioceptive
sensors located in connective tissue to the brain. These proprioceptive sensors
constantly inform the brain about the state of the body. This deficiency would
be related to a malfunction of these sensors in relation to a connective tissue
genetic alteration observed in the vast majority of these patients (see page "FND
and Ehlers Danlos syndrome"). Connective tissue ensures the reinforcement of
almost all organs. For this reason, the brain is poorly and insufficiently
informed and stimulated. In return, this creates muscular tensions, pain, and
control disorders of many organs (motor control, functional colopathy, bladder
disorders, vasomotricity, etc...). This lack of cerebral stimulation is also
probably the cause of the fatigue that is present in all these patients,
associated cognitive disorders (work memory, attention, difficulty in finding
words etc.), possible discomfort, by the intermediary of a possible secondary
brain disconnection. This proprioceptive disorder would therefore favour
"dissociative" phenomena as described in the previous model. For this reason,
these patients are predisposed to undergo FND's during a more or less important
and sometimes subtle physical or emotional disturbance. Indeed, the questioning
and clinical examination of patients with FND very often, (about 3 out of 5
patients and even more frequently in fibromyalgia), allows almost always to
highlight elements in favour one of this constitutional fragility of connective
tissue that characterise the syndrome of Ehlers Danlos "hypermobile" (see
corresponding page). In these patients, it is designed to reactivate the
peripheral proprioceptive sensors by peripheral magnetic stimulation and to act
on cerebral connectivity by transcranian central cerebral large field magnetic
stimulation. The predisposing factors of FND would therefore be essentially
somatic in origin, although psychopathological disturbances may aggravate this
predisposition or be the triggering element.